|
At 9 months postpartum, I am now officially able to talk about my early postpartum experience. The first week of having a new baby is the most magical time. Everything slows down so much. Every day is the same, sleeping, nursing, cuddling, watching movies, eating, and drinking. What isn’t constant is your emotions. They are wild. The immense amount of love I felt for Aspen made me cry with happiness at random times. My heart felt as if it could explode at any moment. It all felt so very right, like the last puzzle piece of my soul had been placed. I was in the most amazing time capsule of life, getting to know my little golden girl. However, parts of the first week can also be very challenging. When you have a baby it is also really highlights who in your community is unselfishly there for YOU (the mother). Those that show up to support you in your most fragile state. Unfortunately, it is so common to overlook the mother and her needs, and focus all the attention on the new baby. Meanwhile the mother is in the background mending to her swollen breasts, her sore and bleeding perineal area, and feeling very overwhelmed. Next time you show up to someone’s home to visit their newborn, bring something for the mom too. Baby outfits are NOT gifts for the mother. Instead bring flowers, a gift card for a massage, or some nice soaps. Let her know she is seen. Luckily, I had a couple of people show up in this way, and I am very grateful for them. The following three months (or fourth trimester) were completely different than my first experience with Toren. Firstly, I was bleeding more postpartum than I did with Toren. Unbeknown to me, this is very common after you have already had a baby. Unfortunately, I bled for almost 6 weeks postpartum! I think part of it was my fault. I felt so good mentally and physically (initially), I just wanted to do more than I should have. Slowing down is soooooooo hard for me. As soon as I feel good, I want to do all the things. For me, walking was so important for my own mental and physical health, but even short, easy walks would leave me bleeding more. So I really had to slow down, and take a break, which was such a struggle…. At about two months postpartum, I started to develop some insomnia, which led to a very sleep deprived mama. I became so dizzy, had vision problems, and felt extremely lightheaded from the lack of good quality sleep, that I was afraid to drive and even went to the doctor worried about more severe issues. Everything the doctor tested came back normal (and optimal in my book)– thyroid, iron panel, CBC, CMP etc. “You are just tired and stressed new mom dear”, she said. “Take some more time for self-care”. Annoyed by her answer I also ordered some additional labs on my own, including a 4 point salivary cortisol test, plasma zinc, vitamin A (retinol), vitamin D, RBC magnesium, copper, and ceruloplasmin. My cortisol levels came back functionally low indicating I was dealing with burnout. No surprise there based on the lack of quality sleep I was dealing with and increased stress from navigating my new life with two kiddos (including a very jealous preschooler). The most surprising result was how low my plasma zinc levels were. I was deficient in my book, and almost deficient based on standard lab testing. Yikes! That was the answer to my sleep issues. Not that a breastfeeding infant helps with that. BUT I was likely struggling to fall asleep, and fall back asleep after I nursed Aspen because of this deficiency. Did you know that a zinc deficiency can impact sleep quality because it plays a very important role in making melatonin? Plus, zinc helps regulate cortisol and we use up a lot of zinc under times of stress. It is also not uncommon for women to develop zinc deficiencies during pregnancy and postpartum due to the increased demand for zinc. Furthermore, zinc deficiencies are correlated to postpartum depression (PPD), and supplementation thereof has helped improve postpartum mood scores and reduces the risk of developing PPD. Although my diet contains zinc rich foods, based on my symptoms and my lab results, I then made a decision to supplement with zinc picolinate at a dose and frequency ideal for my case. I also increased my vitamin A intake via liver/liver pate and added a little extra vitamin D to help boost my levels to more optimal ranges. In addition, I took some ashwagandha and lemon balm tinctures to help manage my stress. Within 30 minutes after taking the tinctures my brain fog cleared, my dizziness went away, my energy increased, and I felt like my normal self again. It was such a relief! After a week of taking the zinc I also noticed that my appetite improved and slowly my sleep patterns improved as well. I relied less and less on melatonin for support and now, unless I work at night, I can fall asleep easily and can fall back asleep quickly. Phew! Now, I just need to do some repeat blood work again, and a hair tissue mineral analysis, just to make sure all is balanced in its right place. In retrospect, I am so glad I KNOW all this stuff and have access to lab testing as a functional dietitian. If I didn't know all this, then gosh, I would have been miserable for so much longer. So please, please, please, advocate for yourself! If you are a postpartum mama out there, don't let miserable symptoms be chalked up to “you're just a new mom and stressed”. With that said, please do not go out and supplement with zinc on your own without knowing your levels. Too much zinc can also cause issues of its own. Work with a qualified practitioner to help match your symptoms with your lab results, and put together a protocol to fit YOUR needs. Around 5 months postpartum after a bout of significant stress (transitioned to solo parenting for the season and decided to take the kids camping), I broke out in a huge cold sore on my chin. Interestingly this happened with Toren as well around the same time when I returned to work. Unfortunately, my cold sore this time around is taking a lot longer to heal. It even reactivated after a second episode of intense stress a month later and still hasnt cleared up completely. This was a blatant reminder for me that breastfeeding and caring for a new baby is a HUGE stressor on my body, and that tipping the scale just a tad too much can result in a wide variety of symptoms. For me it was initially insomnia and then the cold sore. For others it may be postpartum depression or anxiety, developing an autoimmune thyroid disease, etc. It is such a vulnerable time for new moms and unfortunately, the support still lacks greatly...especially in the later postpartum phase.
Unexpectantly, my period came back much earlier than with Toren. I started at around 5 months, instead of 9 months. I swear taking the zinc picolinate triggered an earlier start. When I am not as consistent with it, I skip, and when I am more consistent, I get another period. I have a theory that zinc status may reflect when a mama starts her period again postpartum. Makes sense to me based on all the roles zinc plays in hormone production. Anyways... Otherwise, the rest of my postpartum experience with Aspen has been good. She nursed exclusively for the first 6 months. I did get fitted for my breast pump very early on with a lactation consultant to help make pumping more enjoyable and efficient. Did you know that standard breast shields/phalanges are much too big for the average female? And they make pumping more uncomfortable and less efficient? Yep. Get fitted ladies. Forunately, I never had an event where I was forced to be away from Aspen for a long period of time that required more than one feed from frozen milk. Therefore, I never pumped extra for a "freezer stash" because I didnt want to spend extra energy and nutrition to make it. My body was already needing so much support that I wanted to give my baby and myself all that energy and nutrition and not have it go to waste in the freezer. I personally only have about 2-4 extra bags in the freezer at any given time that I first started when my milk came in early postpartum. I pumped for relief until supply eased up. Since then I replace what is used keeping my frozen milk pretty fresh and up-to-date with my infants needs. I did the same with Toren. At 6 months I started to introduce solids to Aspen, using a combination of baby led weaning and purees. Solid Starts is a great app you can download for guidance on baby led weaning. When I have the time, I also prefer to make my own protein and fat rich purees to give Aspen. For more information about baby food, check out my article here. Now, at 9 months postpartum, I am feeling great despite still having very interrupted sleep. Unfortunately, Aspen wakes up at least two times a night to feed, unlike Toren who slept through the night at 6 weeks postpartum (such a dream). With two kiddos in tow, there is never a quiet moment, until the evening when both are asleep and I can finally catch an hour or two to knit or just relax. Also, now I get to rejoice in the regrowth of baby hair. For a minute there I was getting worried I was going bald! But alas, now I just have 2 inch hairs sticking up around the top and sides of my face...haha! Oh what a ride motherhood is! It keeps you humble thats for sure. Note: if you haven’t read my second pregnancy recap, deficiently check out that article here. Outline of Things I did to Support my Postpartum Period IMPORTANT DISCLAIMER: This is not medical advice. This is what I did based on my unique needs. Please talk to your health care professional and/or dietitian to see what is right for you.
0 Comments
Continuous glucose monitors are becoming all the rage these days. For those of you who are new to CGMs, they check your blood sugar every 5 minutes for about 10 days. With such frequent testing, without having to prick your finger over and over again, you are able to see real time data on how what you are eating NOW impacts your blood sugar.
Why should you care? Repeated suboptimal elevations in blood sugar levels can lead to inflammation and promote cellular aging. High blood sugar levels leads to the production of advanced glycation end products, otherwise known as AGEs which can lead to chronic health conditions and accelerated aging. Excessive spikes are also a risk factor for developing type 2 diabetes, heart disease, kidney disease, Alzheimer’s, etc. So I decided to try it for myself. Why? Because I love n of 1 experiments and I wanted to see how my dietary choices, my lifestyle, my exercise, and my sleep affected my blood glucose levels. I used a Dexcom G6 for 10 days. The first 5-6 days I ate as I normally would. The remainder of the days I adjusted things to try to achieve what I considered optimal glucose management. Based on research I had done (here, here, here, and here), the goals I wanted to achieve were:
So what did I learn about myself?? Well, that's what is so interesting…I learned a lot! Without the insight of the CGM I would never have this deep understanding of what I can do to tweak things to better control my blood sugar, reduce inflammation and AGEs, and ultimately support optimal health. Here is what I learned:
Overall, what I learned just confirmed what I knew, but also individualized things based on ME and MY current lifestyle. Currently I am a breastfeeding mama of two, that prioritizes quality balanced meals with lots of veggies, that isn’t exercising hardcore (rather just taking long walks most days), and getting VERY bad sleep. This experiment showed me that yes, I can make sure my blood sugars are well controlled if I am more mindful of my food choices and my exercise, despite having very poor quality sleep (which unfortunately negatively impacts insulin sensitivity). Interestingly breastfeeding helps increase insulin sensitivity, so together these two factors are likely a wash at this point for me. So based on this experiment, what will I change?
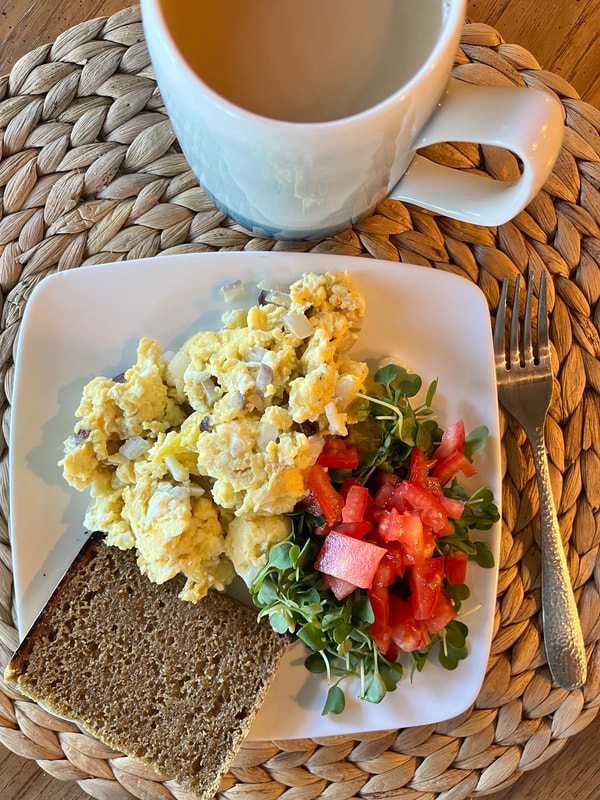
Now I am curious what will happen when I stop breastfeeding and my sleep quality improves… Maybe then I will reach for another CGM experiment! And just for those of you who are curious, the pictures below are a fews of the meals and snacks that met all my blood sugar goals. Planning and Preparing for My Second Pregnancy As a commercial fisherman’s wife whose husband is gone April through September, I have to plan my pregnancies. There really is only a very short window of time to conceive. Once we finally decided that we did indeed want a second child, we opened up January, February, and March 2022 as potential conception months. If we didn't get pregnant during that three month window we decided we would only have one child. But alas, luck was on our side and we got pregnant in February, honestly the perfect month. That gave us a due date of November 13th, neither too close to Dane’s homecoming in October nor right in the midst of the holidays. A November baby would allow us to have plenty of time together as a new family of four before my husband would have to leave again. My pregnancy spacing of three years was very intentional. I wanted to fully recover my nutrient stores after a 22 month breastfeeding journey with my first kiddo and regain full strength in my pelvic floor. Plus, I thought having a more independent preschooler would hopefully make the solo parenting of two kids a tad easier?? Luckily as a dietitian I have access to tools to easily assess my nutrition status including a comprehensive micronutrient test through Vibrant America and a hair tissue mineral analysis through Trace Elements Lab. Furthermore, I check some maintenance labs 1-2x per year just to make sure everything is on point. I offer all this testing to clients of Happy Belly as well. Lab Testing & Wellness Support Prior to getting pregnant I had already been working on addressing nutrient deficiencies (zinc, K2, and coQ10, as well as other nutrients that were in suboptimal range) that I had tested a year prior via diet and supplementation. Then in January 2022 I ordered a hair tissue mineral analysis (HTMA) test to check my mineral status and my nervous system state. The results highlighted that I was low in my macrominerals magnesium, calcium, potassium, and sodium, and that I needed to really focus on managing my stress. Based on the results I started back up on my magnesium supplement and became very intentional about my dietary calcium, sodium, and potassium sources to ensure I met my needs. Both of these tests are great tools to complete at any time in your preconception journey. At the beginning of my first trimester I also ordered my own personal blood labs including full thyroid and iron panels, CBC, CMP, vitamin A, vitamin D, vitamin B12, folate, RBC magnesium, copper, ceruloplasmin, and zinc. The results highlighted suboptimal vitamin A, magnesium, and zinc levels. With the above blood lab results along with my HTMA results I was able to implement my own unique food and supplement routine. Along with addressing my nutrient status and stress levels, I went to see Dr. JoAnne at Rooted in Wellness Chiropractic. She uses more tonal chiropractic techniques along with diagnostic tools to test your sites of muscle tension and your current nervous system state. With her adjustments and my individualized nutrition support I was able to recalibrate my nervous system to be the best she has seen. I continued to see her throughout my entire pregnancy to support my alignment and overall wellness. I highly recommend that anyone local to Bellingham reach out to her as well! Pregnancy Journey Otherwise, my second pregnancy was very similar to my first. No complications and no real complaints. I also gained similar amounts of weight with each, about 25-30lbs. During my first trimester I did experience some mild nausea and fatigue during weeks 6-8, but that cleared up pretty quick. Eating balanced meals, with a big focus on protein rich foods, really helped keep my blood sugars stable and my nausea and fatigue within control. I also had some mild constipation, but I knew how to keep things moving. In addition to a whole foods diet rich in fiber, I focused on drinking plenty of coconut water and enjoyed a variety of papaya, kiwi, chia seeds, and Nancy’s Probiotic yogurt daily. The second trimester went by really fast, it was summer after all. I intentionally reduced my client load, and tried to find more “quiet solo time” usually as a nature walk. Throughout my entire pregnancy I made sure to walk every day if possible. My daily goal was 3 miles. Sometimes it was more, sometimes it was less. And sometimes, I didn't get any “real” movement in, and that was okay too. I tried to give myself grace when it didn't work out like I intended. Honestly, pregnancy and postpartum are the most important times in your life to try and chill out. The harder you work, and the more you add to your list, the more you dig yourself a hole. So please, don't try to do it all. If you can take things off your list, reduce your exercise intensity if you are used to pushing yourself hard, and find some time to just relax. During my mid second trimester I also repeated my blood labs and completed another HTMA test to see what dietary and supplement adjustments I might need to make. Magnesium levels dropped a little bit (not surprisingly because pregnancy increased magnesium demand so much), so I increased my magnesium supplements again from 240mg to 360mg and took them every day religiously before bed. The third trimester was smooth sailing as well. I tested negative for gestational diabetes and Group B Strep. Woohoo! However, based on current classifications of anemia during pregnancy (hemoglobin <11g/dL), my labs at 27 weeks indicated “slight anemia” at 10.9g/dL. Currently there is much debate in the medical field around classifying anemia with a cut off of <11g/dL or <10.5g/dL. Many argue that 10.5g/dL should be the true cutoff point due to the natural hemodilution that happens in the late second trimester and early third trimester. Therefore, I declined the three IV iron infusions that were suggested by my nurse midwife and instead continued to focus on eating 2-3oz of liver per week and eating grass-fed red meat almost daily. I only supplemented with a small dose of easy to digest iron bisglycinate (28mg) occasionally when I did not eat liver or red meat, which was about 2x per week because my prenatal did not contain any iron (which is intentional). I am very cautious with iron supplementation as there are both benefits and risks to assess and personally don't agree with blindly supplementing high dose iron or IV iron infusions unless there is a true need. Generally speaking “mild” cases of anemia (hemoglobin of 10 - 10.9g/dL per WHO) respond beautifully to dietary interventions and do not need high dose iron replacement or iron infusions. Normally over the course of the third trimester hemoglobin levels rise naturally from their lowest levels around 24-30 weeks of pregnancy. So if hemoglobin levels were fine all throughout your first and second trimesters, and then dip, know that they will start increasing again at 33 weeks. If you start your pregnancy with a hemoglobin of <12g/dL you may need earlier interventions (food first, then supplementation) to avoid more moderate or severe anemias later on in pregnancy. As you can see, iron metabolism during pregnancy is much more complicated than just replacing iron. Along with normal hemodilution during the third trimester, there are other nutrients of concern, including vitamin A and copper which play an essential role in iron metabolism that unfortunately are never tested for or mentioned in the traditional health care model. Furthermore, in addition to checking vitamin A and copper, testing a full iron panel along with ferritin instead of just hemoglobin is ideal to assess true iron need. So please, work with a skilled dietitian to help guide you throughout your unique journey. And just to note, with my food focused interventions and the natural increase in hemoglobin concentration my hemoglobin levels were at 13g/dL at the time of delivery. No IV infusions needed and no harsh ferrous sulfate supplements. Yay for self-advocacy! Birth Since I was considered a “geriatric pregnancy” this time around, I did have more ultrasounds and weekly non-stress tests during the last four weeks of my pregnancy. Luckily the results all came back great and I was able to push back the suggested 39 week induction to the middle of my 40th week. I hoped I wouldn't need it. I hoped that the baby would come before 40 weeks just like my son Toren. But alas, my journey this time around was not the same. At 40 weeks and 4 days, I was admitted to Peace Health Child Birth Center to start my induction process. After a week of processing high and low emotions, and the wonderful support and guidance of a dear friend, I arrived at the Child Birth Center feeling very grounded, empowered, and ready. Ready to have an amazing labor. I left fear behind me, and entered with such presence. I had an amazing team ready to help me have the best experience - my nurse midwife, two awesome Labor & Delivery nurses, and of course my amazing husband. Since I was only 2cm dilated my induction process started with Cervidil – a cervix ripening prostaglandin that is inserted vaginally. My midwife said, “We will wait 4 hours, and then check how far you are at that point. If you are 3cm or more, then we can start Pitocin”. With four hours of waiting time, my nurse helped me through a Miles Circuit (to help get baby in the best position) and she massaged my hips to help release and relax my ligaments. I also got to enjoy a steaming hot bowl of delicious Pho and a side of diced papaya and lime that my husband brought me for lunch. And then it was go time. At 1pm my midwife checked me again and said, “You're at 3 cm, we can start Pitocin or do another round of Cervidil”. I asked the nurse what dose is usually required to help kickstart labor for women and she said that it ranges between 8ml/min to 20ml/min. I opted for Pitocin, and jokingly said “Hopefully I will only need a little Pitocin Kiss to get going”. With Pitocin they generally start at 2ml/min and increase by 2ml every 30 minutes until contractions start to get intense. With the first 2ml, I noticed gentle contractions. By 4ml/min I had to do some breathing through them, and by 6ml/min I was groaning through my contractions and moaning my mantras “Opening”, “Releasing”, and “Sensation”. When the nurse came in to check in on me at 4:30pm my water broke. It felt like a water balloon had popped inside me. Then things got really intense fast. They started to titrate the Pitocin back down again, and eventually weaned me off. So indeed all I needed was a little “Pitocin Kiss” to get my body to do its own thing. At 5pm they checked me and I was at 5cm. With the support of my amazing husband I continued to labor another hour with my mantras and deep groans and relaxed in between contractions with deep breathing, cold wash cloths, and the loving touch of my husband. At 6pm I hit transition, the intense contractions that leave you shaken to your core. I was checked again and I was at 9.5cm. “You’re ready to start pushing!” said my midwife. And so I did, surrounded by my amazing support team. After 20 minutes, my husband caught our 8lb 2oz baby and announced that it was a girl – the most amazing blessing I could have ever asked for! My little golden girl Aspen finally made her debut. She immediately came to my chest, latched to my breast right away, and the cord clamping was delayed at least 5 minutes if not longer (time has no meaning so it’s hard to know exactly). I was so in love, so blissed out, and so extremely happy. I did it! I was 200% there mentally, emotionally, and physically…and for an extra bonus I didn't even tear. Phew! Although I was much more present with myself this time around, I felt much more disconnected with this pregnancy. I have talked to many mamas and most agree they felt the same. Life is much busier when you have another kiddo in tow while you are working and pregnant. It’s also not your first rodeo. The “new” excitement isn’t there. You have been there done that already. I also struggled with an intense worry that I wouldn't be able to love my second child as much as I loved my first. But trust me….this is NOT something you need to lose brain cells on. Aspen has shown me that your heart can grow twice as big to allow for so much more love than you could have ever imagined. And now as a family of four we navigate the change of pace and adjust to the ebbs and flows of this wonderful journey. My Second Pregnancy Tools, Diet, and Supplements: IMPORTANT DISCLAIMER: This is not medical advice. This is what I did based on my unique needs. Please talk to your health care professional and/or dietitian to see what is right for you.
Stay tuned for my postpartum update!
Potassium is a macromineral that plays a big role in supporting optimal GI function. Unfortunately, 98% of Americans are not getting adequate amounts of potassium in their diet due to inadequate fruit and vegetable intake. Fad diets that remove fruit and starchy veggies like potatoes and squash, as well as avoid quality dairy, increase the risk of inadequate potassium intake. Furthermore, individuals may lose potassium due to potassium wasting medications (like diuretics), high coffee or alcohol intake (also diuretics), excessive sweating from high intensity exercise or sauna, and high levels of stress (hello COVID years!). Why is it important to focus on potassium intake?? There are many reasons why focusing on potassium intake can benefit your health. But today I want to focus on two directly related to gut function.
For healthy individuals aim for 3500mg or more of potassium per day. If you are unsure how much potassium you are getting daily, I highly recommend tracking your food intake for three days on Cronometer. Get an average, and see how close you are to getting 3500mg per day, then make some dietary changes or tweaks to boost that level. Some potassium rich foods are listed below. You can also check out this awesome source listing out the top 100 potassium rich foods.
If you are a SIBO or IBS patient and are on a limited diet consider adding in the following low FODMAP, high potassium foods.
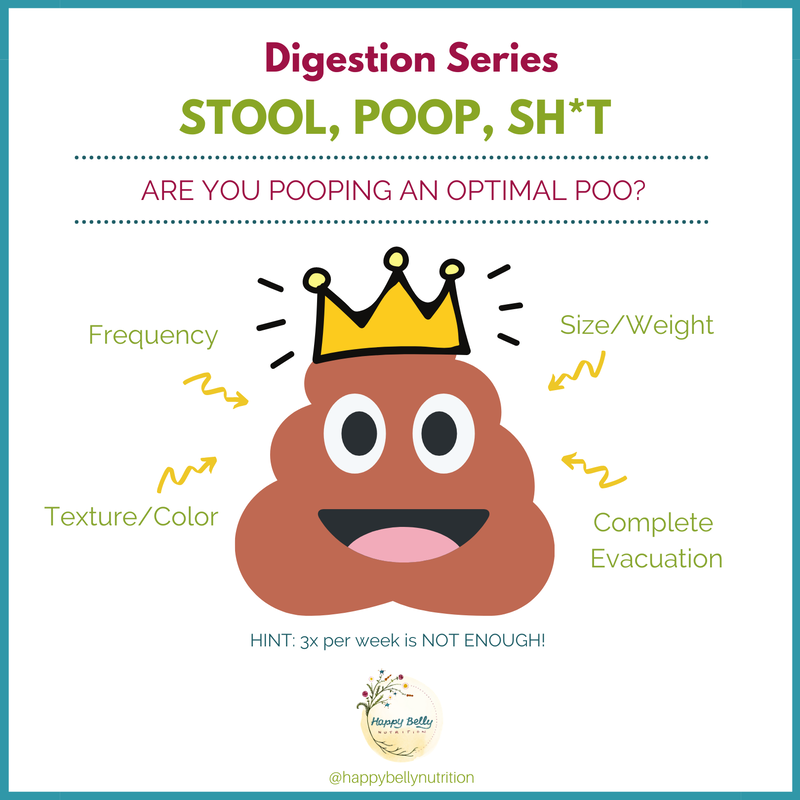
NOTE OF CAUTION: If you have kidney disease or are taking potassium sparing medications (including spironolactone, amiloride, eplerenone, triamterene, etc) work with your health care provider because you may need to REDUCE your potassium intake and not increase it. How many times should we poop a day or a week?? What should a healthy poop look like? This unfortunately can be kind of hard to study because most people don't really think about their poop much nor do they know what is considered normal. So when asked in a survey to describe their bowel frequency and texture, some people may not even really know how to answer these questions. Do you know?? Unfortunately, WE DON'T TALK ABOUT POOP ENOUGH. Granted, it’s not the best table talk (unless of course you’re out to dinner with a group of dietitians), but it is something we all need to be aware of and educated about. A recent study in 2017 studied the US population via a survey asking these exact questions. How often do you poop each week and what does it look like (based on the Bristol stool chart). Here is what they found: 3% have < 3 poops per week 60% have 3-7 poops per week 30% have 8-14 poops per week 6% have 15-21 poops per week 1% have >21 poops per week They also found that normal poops happen more often in men than women, in those with a higher education and income, in those requiring less medications (<2 per day), and in those who eat more fiber (>20g per day). Based on the above results, researchers concluded that normal for the US population is considered at least 3 poops per week up to 3 poops per day. However, this doesn't really highlight the other considerations of what is considered a healthy bowel movement such as the texture of the poop (is it firm, sticky, loose, pebble-like), the stool weight (how big is it), or the sense of complete evacuation (do you feel empty afterwards?). Another study of Coastal Indians, who eat a predominately plant based diet, found that the average stool frequency was 14 poops per week, mostly resembling an easy to pass smooth banana. They also found that vegetarians and more physically active individuals tended to pass stool more frequently. Average stool weight in Asia is also much higher than that of a Western populations, with an average of 311g per 24 hours. Stool weight in many Western populations is low (80-120g per day) which is associated with an increased risk of colon cancer. Stool weights of 150g per day can help reduce this risk.
So what is considered optimal?? Clinically, I do not agree with 3x per week! The Western population as a whole is not eating enough fiber. If you look at other higher fiber eating populations, they average 2 poops per day, with an average poop weight of 150g. This translates to TWO LARGE, firm but not hard, easy to pass, bowel movements per day. I also see this in my clients. When they are pooping 2x per day, they feel good, they look good, and they are happier. So just because you are pooping every day, it does not mean your poop is considered optimal. If you are concerned about your pooping habits, work with a gut health dietitian (like me!) |
AuthorLike to read? Then get your evidence based nutrition information here! All posts written by Selva Wohlgemuth, MS, RDN Functional Nutritionist & Clinical Dietitian Archives
August 2023
Categories
All
|
Providing custom functional nutrition therapy since 2015.
Follow HBN on Social Media!
©Happy Belly Nutrition, LLC 2015-2023
Proudly powered by Weebly






























 RSS Feed
RSS Feed


